Trauma-informed care in child/family welfare services
February 2016
Liz Wall, Daryl Higgins, Cathryn Hunter
Download Policy and practice paper
Overview
This paper aims to define and clarify what trauma-informed service delivery means in the context of delivering child/family welfare services in Australia. Exposure to traumatic life events such as child abuse, neglect and domestic violence is a driver of service need. Policies and service providers must respond appropriately to people who are dealing with trauma and its effects in order to ensure best outcomes for individuals and families using these services. In addition to evidence-based programs or clinical interventions that are specific to addressing trauma symptoms, such as trauma-focused cognitive behaviour therapy, there is a need for broader organisational- or service-level systems of care that respond to the needs of clients with a lived experience of trauma that go beyond a clinical response. Some of the challenges identified in implementing and embedding trauma-informed care across services and systems are discussed.
Key messages
-
Traumatic experiences are common, with people often having multiple adverse experiences across their life. There are many serious and deleterious outcomes associated with exposure to them.
-
Clients often present to child/family welfare services with a complex range of symptoms and behaviours related to prior and/or past trauma, which neither they nor those working with them have linked to this previous trauma exposure. As a result they may face an uninformed and fragmented response that is potentially re-traumatising.
-
There are a small number of trauma-specific interventions that have been evaluated using a rigorous scientific standard and been shown to be effective - however, the research is often based on populations who have experienced a single traumatic event rather than complex trauma.
-
Trauma-informed care is a framework for human service delivery that is based on knowledge and understanding of how trauma affects people's lives, their service needs and service usage.
-
With the lack of an overarching framework in Australia, there is a danger of inconsistent or piecemeal development of trauma-informed models and practices that do not share a consistent language or framework for implementing trauma-informed systems of care in child/family services.
Introduction
Understanding the experiences of adversity in childhood such as sexual or other abuse as trauma is now recognised to be an important concept for human service delivery sectors. The USA has led efforts to incorporate trauma theory into mental health and other service delivery, largely driven by the Substance Abuse and Mental Health Services Administration (SAMHSA). SAMHSA funds two major trauma-related resources, the National Center for Trauma-Informed Care (NCTIC) and the National Child Traumatic Stress Initiative (NCTSI), to provide a focus for developing a shared language and evidence base around trauma and trauma-informed approaches to service. Emerging efforts in Australia are now contributing to our knowledge of effective practice for children, young people and adults who have experienced trauma from events such as child maltreatment, sexual assault, military service, forced adoption and past family separation practices.
This paper aims to define and clarify what trauma-informed service delivery means in an Australian context. Australia is not as far down the track as the USA in terms of implementing a trauma-informed approach to human service provision in systems such as mental health and child and family services. There is, however, a recognition that exposure to traumatic life events is a driver of service need and that policies and service providers must address and respond to trauma appropriately to ensure best outcomes for individuals and families using these services.
Trauma terminology
There has been extensive debate around the classification and terminology for describing the effects of trauma, as well as the relationship to specific diagnostic terms such as post-traumatic stress disorder (Van der Kolk, Roth, Pelcovitz, Sunday, & Spinazzola, 2005; Wall & Quadara, 2014). The latest iteration of the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013), an international classification system for mental health disorders, has taken a broad approach to the terminology with a category of "Trauma and Stressor Related Disorders" rather than specifically including complex trauma as a diagnostic term.
Any discussion of trauma-informed service delivery requires consideration of the vast array of definitions and terminology that arises around trauma. This section explains some of the different terms, phrases and concepts that are used in the literature to describe trauma and trauma-related service provision.
Recently, there have been attempts to provide consistency in definitions and a shared language around trauma and a trauma-informed approach to care. SAMHSA's (2014) Concept of Trauma and Guidance for a Trauma-Informed Approach puts forward definitions and a working concept of trauma and a trauma-informed approach in order to develop a shared understanding of these concepts for service systems and stakeholders. SAMHSA is a key resource for trauma-informed approaches to care and these definitions are likely to be widely adopted.
What is trauma?
Traumatic events have been described as those that "overwhelm the ordinary human adaptations to life [and] … generally involve threats to life or bodily integrity, or a close personal encounter with violence and death" (Herman, 1992, p. 33). SAMHSA's concept of trauma provides a comprehensive definition that encompasses trauma related to one-off events as well as ongoing adversity:
Individual trauma results from an event, series of events or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting adverse effects on the individual's functioning and mental, physical, social, emotional or spiritual wellbeing. (SAMHSA, 2014, p. 7)
Although not diagnostic terms, complex trauma and complex post-traumatic stress disorder are often used to describe trauma that is the result of stressors that are interpersonal - usually severe, sustained and perpetrated by one human being on another - and where clients may not meet all of the specific diagnostic criteria for post-traumatic stress disorder (PTSD) or where the primary clinical presentation is the associated features due to the global effects of trauma on the person's functioning (Connor & Higgins, 2008a, 2008b). Trauma is particularly damaging when it occurs in childhood. Complex, interpersonally generated trauma is severely disruptive of a person's capacity to manage internal states (Kezelman & Stavropoulos, 2012). Complex trauma symptoms include problems with mood regulation, impulse control, self-perception, attention, memory and somatic disorders (Briere & Jordan, 2004; Burstow, 2003; van der Kolk et al., 2005).
Trauma-informed interventions occur at two levels: trauma-specific interventions and trauma-informed models of care. Organisational responses to trauma tend to occur on a continuum from basic trauma awareness, to trauma sensitivity, trauma responsivity and through to trauma-informed and/or trauma-specific interventions. We argue here that it is helpful for organisations providing services in the child/family welfare domain, and human services more broadly, to think about their organisational responses to trauma based on their particular service and client needs.
Trauma-specific interventions
Trauma-specific interventions refer to clinical services or programs designed to treat and ameliorate the actual symptoms and presentations of trauma. While it is possible for individual practitioners to deliver trauma-specific interventions (such as trauma-focused cognitive behaviour therapy [CBT]) within the context of a service delivery model or agency that is not trauma-informed at a system level, this is far from ideal. Elements of a service may not be consistent with a trauma-informed approach - such as the waiting room design and operation, interactions with administrative staff or the absence of adjunct services to address other presenting issues for which the trauma-specific intervention might not be effective. Trauma-specific services are best delivered as part of a trauma-informed system of care operating within a trauma-aware organisational context (Elliot, Bjelajac, Fallor, Markoff, & Reed, 2005; Kezelman & Stavropoulos, 2012).
Funded by the Department of Veterans' Affairs, Phoenix Australia (previously known at the Australian Centre for Posttraumatic Mental Health) has developed a database that summarises the evidence for effective trauma-specific interventions related to military and veteran families and communities (see What Emerging Interventions are Effective for the Treatment of Adults with PTSD? Regarding adults suffering from PTSD, they found a paucity of evidence in relation to the efficacy of emerging therapies.1 Phoenix Australia have also published a variety of resources for practitioners working with people affected by trauma, including fact sheets, clinical guidelines, booklets for clients and a smartphone app for clients with post-traumatic stress symptoms.
Trauma-focused cognitive behaviour therapy (TF-CBT) is an evidence-based treatment approach for children who have experienced sexual abuse, exposure to domestic violence or similar traumas.2 TF-CBT features on a range of databases of evidence-based practices, including the California Evidence-Based Clearinghouse for Child Welfare (CEBC) Program Registry. Training in TF-CBT is available online from the Medical University of South Carolina website. However, a full discussion of evidence-based trauma-specific interventions is beyond the scope of this paper.3
Similarly, in relation to adults affected by childhood trauma, Connor and Higgins (2008a, 2008b) outlined a model of trauma-specific intervention for clients who experience complex trauma (who may not meet the criteria for PTSD). Evaluating the model, they found qualitative and quantitative evidence from a small-scale pilot study of the effectiveness of their combined individual and group therapy approach focused on the following elements (using the mnemonic "HEALTH"):
- having a supportive therapist;
- ensuring personal safety;
- assisting with daily functioning;
- learning to manage core PTSD symptoms (self-regulation);
- treating complex PTSD symptoms; and
- having patience and persistence to enable "ego strengthening".
However, there have been criticisms made of trauma-specific interventions. For example:
- complex trauma is often inter-relational in nature, so the degree to which research on the treatment of combat-related PSTD applies in these circumstances has been questioned (e.g. for those exposed to prolonged child sexual abuse, particularly if it has resulted in personality or dissociative disorders and is associated with disturbances to affect regulation, self-concept and interpersonal relationships);
- treatment sessions may need to be more frequent and over a longer duration than typical structured programs;
- evaluations of cognitive-based interventions often focus on statistically significant effect sizes rather than clinically meaningful symptom reduction; and
- the value of non-cognitively based interventions, which have been poorly evaluated or not evaluated, are easily overlooked (see: van der Kolk, 2014).
The primary purpose of the paper is not to review the effectiveness - or limitations - of trauma-specific interventions, or even to look specifically at complex trauma and complex PTSD (see: Wall & Quadara, 2014); but rather to explore the broader issue of the value and role of trauma-informed care in child and family welfare service provision.
Trauma-informed model of care
The available literature suggests that there is a continuum from being trauma aware (seeking information out about trauma and its implications for organisations) to being trauma-informed (a cultural shift at the systemic level). One useful resource sets out the progression in four stages (see Figure 1):
- trauma aware: seek information out about trauma;4
- trauma sensitive: operationalise concepts of trauma within the organisation's work practice;
- trauma responsive: respond differently, making changes in behaviour;
- trauma informed: entire culture has shifted to reflect a trauma approach in all work practices and settings.
Figure 1: Practical steps to get from trauma aware to trauma informed
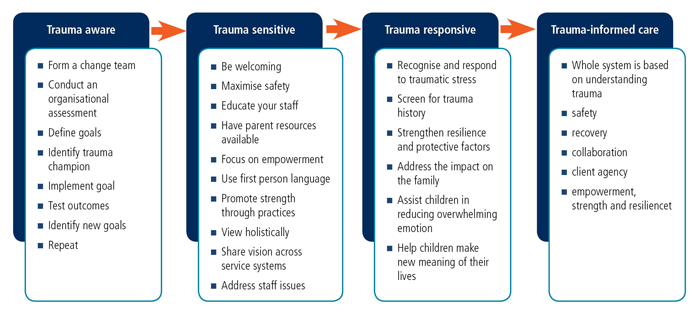
Source: Adapted by Antonia Quadara from Mieseler & Myers (2013)
SAMHSA's definition of a trauma-informed approach to service is:
A program, organisation or system that is trauma-informed realises the widespread impact of trauma and understands potential paths for recovery; recognises the signs and symptoms of trauma in clients, families, staff and others involved with the system and responds by fully integrating knowledge about trauma into policies, procedures and practices and seeks to actively resist retraumatisation (SAMHSA, 2014, p. 9)
The main aim of this paper is to explore trauma-informed approaches to care and service delivery specifically in the child and family welfare sectors. While the focus is on how child/family welfare services can be trauma informed, the need extends to other service delivery areas. The trauma literature indicates that trauma survivors are clients in a very broad range of human services such as:
- homelessness (Hopper et al., 2010; Morrison 2009);
- mental health (Kezelman & Stavropoulos, 2012; Muskett, 2014);
- substance abuse treatment; and
- correctional systems (Stathopoulos, 2012).
These types of services have a clear connection to the impacts of trauma, particularly trauma arising from interpersonal victimisation, which has been identified as a driver of human service use (Huntington, Moses, & Veysey, 2005). The term "complex needs" is sometimes used to describe the span of need for an array of services required over a lifetime (Wall & Quadara, 2014). These agencies and services would benefit from being - at a minimum - "trauma aware".
1 The emerging interventions included in their review were: mindfulness, acceptance and commitment therapy, meditation, transcendental meditation, acupuncture, power therapies, and experiential psychotherapies including adventure therapy, art therapy, music therapy, and canine- and equine-assisted psychotherapy. See: <evidencecompass.dva.gov.au/home/question/10>.
2 See: Trauma-Focused Cognitive Behavioral Therapy for Children Affected by Sexual Abuse or Trauma(Child Welfare Information Gateway, 2012) <www.childwelfare.gov/pubpdfs/trauma.pdf>.
3 See Approaches Targeting Outcomes for Children Exposed to Trauma Arising From Abuse and Neglect: Evidence, Practice and Implications (Australian Centre for Posttraumatic Mental Health & Parenting Research Centre, 2014) for a discussion of the evidence of the effectiveness of trauma-specific and trauma-informed practices pertaining specifically to children who have experienced abuse and neglect.
4 At its most basic level, organisations that are trauma aware incorporate trauma awareness into their work. Staff have an understanding of trauma and how symptoms and behavioural presentations in individuals may be responses to traumatic experiences so that behaviours that appear self-destructive or self-defeating can be acknowledged as being adaptive behaviours to trauma that have become maladaptive over time (Hopper, Bassuk, & Olivet, 2010; Markoff, Fallot, Reed, & Elliot, 2005). This applies particularly to broader human service delivery agencies (beyond child/family welfare), particularly if they are not primarily focused on delivering trauma-specific interventions and/or trauma-informed models of care.
What is the evidence that a trauma-informed approach is needed?
Research suggests that exposure to adverse, potentially traumatic events in childhood is not uncommon (Anda et al., 2006). For example, the Adverse Childhood Experiences (ACE) study in the USA showed that of 17,337 respondents, 64% had experienced at least one adverse experience5 and approximately 12% had experienced four or more in the first 18 years of life (Anda et al., 2006). Further to this, a recent report suggested that childhood trauma affects an estimated five million Australian adults (Kezelman, Hossack, Stavropoulos, & Burley, 2015). There is also a great deal of evidence associating traumatic experiences with a broad range of deleterious outcomes in childhood, adolescence and adulthood (e.g. Anda et al., 2006; CFCA, 2014a, 2014b; Dube et al., 2001; Hahn Fox, Perez, Cass, Baglivio, & Epps, 2015; Johnson-Reid, Kohl, & Drake, 2012; Nurius, Green, Logan-Greene, & Borja, 2015).
Individual responses to traumatic experiences vary widely, with not all exposure leading to negative outcomes. It is the individual response to the experience that determines whether it is considered traumatic or not (SAMHSA, 2014). If effects occur they can be short- or long-term and may occur immediately following exposure to adversity or have a delayed onset (SAMHSA, 2014).
Multiple studies have reported negative effects associated with experiencing trauma across all facets of life. Mental ill-health, physical illness, social and relational difficulties, and poor academic and employment outcomes have all been linked to previous traumatic experiences. Anda and colleagues (2006) found a strong relationship between increased numbers of adverse childhood experiences and increased prevalence and risk of:
- affective disturbances (e.g. panic attacks, anxiety, hallucinations);
- somatic disturbances (e.g. sleep disturbance, severe obesity);
- smoking, illicit drug use, injected drug use, alcoholism (for people with four or more adverse childhood experiences);
- early intercourse, promiscuity and sexual dissatisfaction;
- impaired memory of childhood; and
- high perceived stress, difficulty controlling anger and risk of perpetrating intimate partner violence (for people with four or more adverse childhood experiences).
Further to this, the study found that as the number of adverse childhood experiences increased so too did the average number of co-occurring negative outcomes (Anda et al., 2006). There is strong evidence to indicate that certain types of trauma rarely occur in isolation. Research suggests, for example, that the different child maltreatment types are interrelated: sexual abuse, physical abuse, psychological maltreatment, neglect and exposure to domestic and family violence typically occur in combination with each other. A large proportion of children and young people who experience childhood abuse or neglect are exposed to more than one type of abuse (known as "multi-type maltreatment"; Price-Robertson, Higgins, & Vasallo, 2013). Further to this, other forms of victimisation such as bullying or assault by a peer have often been found to co-occur with child maltreatment (known as "poly-victimisation"; see Finkelhor, Ormrod, & Turner, 2007).
Multiple victimisation experiences across different domains are consistently associated with poorer outcomes than a single adverse or maltreatment experience. Those who experience multi-type maltreatment or poly-victimisation are more likely to experience high levels of trauma symptoms and worse outcomes than those who are exposed to no maltreatment or only one type (Finkelhor et al., 2007; Higgins & McCabe, 2001). Supporting these findings, a recent large scale US study of children in the Illinois child welfare system found that children who experienced both violent interpersonal and attachment-based ("non-violent") traumas within the caregiver system experienced greater difficulties across several areas of impairment (including attention/behavioural dysregulation and self/relational dysregulation) and were significantly more likely to exhibit PTSD-like symptoms compared to children who had experienced neither type of trauma, violent trauma only or non-violent trauma only (Kisiel et al., 2014).
Co-occurring mental health issues and disorders such as conduct disorder and oppositional defiant disorder (in children), PTSD, depression and other affective disorders, borderline personality disorder, somatoform disorders, psychotic and dissociative disorders have commonly been associated with traumatic experiences (Bateman, Henderson, & Kezelman, 2013; Breslaue, 2009; CFCA, 2014a, 2014b; Nurius et al., 2015; van der Kolk et al., 2005). Self-harm and suicide attempts have also been linked with previous traumatic experiences (Bateman et al., 2013; Cozolino, 2010; Dube et al., 2001; Herman, 1992; Johnson-Reid et al., 2012). In one study, Dube and colleagues (2001) reported that any adverse childhood experience increased the risk of attempted suicide by 2-5 fold with the relationship being partially mediated by illicit drug use, depressed affect and self-reported alcoholism.
Those who have had previous traumatic experiences also commonly report physical health issues. For example, in summarising research on the potential effects of trauma exposure, Bateman and colleagues (2013) found that "survivors of child maltreatment were at increased risk of hepatitis, diabetes, heart disease, cancer, a stroke, are more likely to have surgery and are at increased risk of having one or more chronic pain symptoms" (p. 19). The same authors also noted a range of conditions that child sexual abuse survivors were at increased risk of, including irritable bowel syndrome, asthma, arthritis and digestive problems.
In addition, childhood trauma exposure has been linked to involvement with the criminal justice system. A large study exploring adverse childhood experiences of serious, chronic and violent juvenile offenders and juveniles referred to the justice system for single non-violent offences found that every additional adverse childhood event experienced increased the risk of becoming a serious, chronic and violent juvenile offender by more than 35%, even when other known risk factors for violent behaviour were accounted for (Hahn Fox et al., 2015).
Lastly, difficulties in interpersonal relationships are often reported as a result of experiencing trauma (Bateman et al., 2013; Briere & Spinazzola, 2005; Evans & Coccoma, 2014; van der Kolk, 2005).
Although individual responses to traumatic experiences may vary widely, research has found a strong relationship between the degree of risk of experiencing multiple and complex negative outcomes following traumatic experiences and factors such as the age at which the experience/s occurred, the nature of the experience/s (with negative effects being particularly associated with trauma of an interpersonal nature such as child abuse and neglect), and the severity and chronicity of the experiences (Cozolino, 2010; Herman, 1992; Kisiel et al., 2014; National Scientific Council on the Developing Child, 2014 [NSCDC]; Resick et al., 2012; van der Kolk et al., 2005). As noted by Cozolino (2010):
The impact of trauma depends on a complex interaction of the physical and psychological stages of development during which it occurs, the length and degree of the trauma, and the presence of vulnerabilities or past traumas. The impact of chronic trauma becomes woven into the structure of personality and is hidden behind other symptoms, making it difficult to identify, diagnose and treat. (p. 266)
Traumatic events experienced early in life can be extremely damaging to the developing brain. Neural development relies on the interplay of genes and environmental inputs (particularly interaction with primary carers) and early adversity or disrupted attachment relationships that lead to chronic high levels of stress can interfere with key neurobiological development (NSCDC, 2014). Pamela Alexander (2013) suggested that "affective synchronization between mother and child" (p. 45) in carer-infant interactions is crucial for brain development, social development and stress regulation. Early onset, sustained trauma that interferes with this can lead to deficits in multiple domains: dysfunction in fear extinction; affect or emotional regulation; behaviour regulation; learning, cognition and attention; and self and relational dysregulation (Cook et al., 2005; Courtois & Ford, 2009; Evans & Coccoma, 2014; Kisiel et al., 2014; NSCDC, 2014; van der Kolk et al., 2005).
Research has also highlighted that experiencing traumatic events tends to increase the chances of experiencing further traumatic events across the life course. Cozolino (2010) argued that:
Enduring personality traits and coping strategies that emerge in these situations [experiencing early onset, sustained trauma] tend to decrease positive adaptation and increase an individual's vulnerability to future trauma. This can manifest through engagement in abusive relationships, poor judgement, or a lack of self-protection. (pp. 268-9)
Finally, in examining the need for a trauma-informed approach to care it is pertinent to note that in many cases, due to the co-occurrence of problems resulting from experiencing trauma, individuals may find themselves in multiple systems, cycling in and out of specific services over many years to access, for example, treatment for drug and alcohol addictions, support for employment opportunities and therapeutic services for mental illness.
Historically, the underlying factor often linking a constellation of needs together - the history of abuse and its impacts - has not been adequately acknowledged or integrated into these service systems' service responses to individuals (Harris & Fallot, 2001). Further, populations with complex needs are at high risk of falling through the gaps of service delivery systems due to a lack of service co-ordination and the related barriers to service integration (Whiteford & McKeon, 2012). This can mean that clients: are deemed ineligible for services (e.g. cannot engage in mental health treatment until they have "dealt with" their substance abuse issue or vice versa); are expected to separate out their trauma experiences from their service or treatment needs ("we don't deal with trauma in this parenting class"); and experience services systems' responses as re-traumatising.
The SAMHSA-funded Women With Co-Occurring Disorders and Violence Study was a comprehensive 5-year project (1998-2003) across multiple sites, which provided evidence that integrating different services, such as mental health and substance abuse services where there was client need for both, was effective. This study showed that trauma-informed approaches could enhance the effectiveness of mental health and substance abuse services for women with co-occurring mental health and substance abuse disorders (Huntington et al., 2005; Morrisey et al., 2005). A trauma committee for this study also developed an understanding of trauma-informed principles and ways in which mental health and substance abuse service providers could use the approach (Elliot et al., 2005). In the years since the study, further development, debate and discussion has resulted in an expanded evidence base about the effects of trauma and appropriate approaches for services.
5 The adverse childhood experiences measured were three types of childhood abuse: emotional abuse, physical abuse, and contact sexual abuse; and five measures of household dysfunction during childhood: exposure to alcohol or other substance abuse, mental illness, violent treatment of mother or step-mother, criminal behaviour in the household, and parental separation or divorce (Anda et al., 2006, p. 176).
What is trauma-informed care?
Trauma-informed care could be described as a framework for human service delivery that is based on knowledge and understanding of how trauma affects people's lives and their service needs (Harris & Fallot, 2001). This requires consideration of a person's environment beyond the immediate service being provided and of how their symptoms and presentations may be seen as adaptations to trauma rather than as pathologies (Herman, 1992). At the broadest level, trauma-informed care means that services have an awareness and sensitivity to the way in which clients' presentation and service needs can be understood in the context of their trauma history (Knight, 2015). Kezelman and Stavropoulos (2012) noted that trauma-informed health and welfare settings and systems contrast dramatically with traditional settings and systems as they require different ways of operating, and without this understanding, risk re-traumatising service users. Trauma-informed approaches to care could be described as a strengths-based framework that is responsive to the effects of trauma (Bateman et al., 2013).
Principles of trauma-informed care
Principles of trauma-informed care have been articulated in a range of academic literature and guidance publications (Elliot et al., 2005; Hopper et al., 2010; Jennings, 2004; Kezelman & Stavropoulos, 2012; SAMHSA, 2014). These principles vary in length and number depending on the publication but essentially have the same underlying philosophies, that trauma-informed care means services are trauma aware, safe, strengths-based and integrated.
At the very minimum, trauma-informed services aim to do no further harm through re-traumatising individuals by acknowledging that usual operations may be an inadvertent trigger for exacerbating trauma symptoms. SAMHSA's (2014) approach to trauma-informed care makes four key assumptions that must be present as a basis of implementation for trauma-informed care, with a further six key principles to then be applied.
The key assumptions that SAMHSA has identified as needing to be inherent in any trauma-informed approach are based on four "R"s:
- Realisation at all levels of an organisation or system about trauma and its impacts on individuals, families and communities;
- Recognition of the signs of trauma;
- Response - program, organisation or system responds by applying the principles of a trauma-informed approach; and
- Resist re-traumatisation - of clients as well as staff.
In addition to these assumptions, SAMHSA (2014) then described six key principles of a trauma-informed approach:
- Safety - Staff and the people they serve feel physically and psychologically safe.
- Trustworthiness and transparency - Organisational operations and decisions are transparent and trust is built.
- Peer support - Peers is the terminology SAMHSA use for individuals with lived experience of trauma or their caregivers. Peers are also known as "trauma survivors".
- Collaboration and mutuality - This principle is about levelling power differentials between staff and clients and amongst organisational staff to ensure a collaborative approach to healing.
- Empowerment, voice and choice - This principle emphasises the strengths-based nature of trauma-informed care. The organisation - and ideally the whole service delivery system - fosters recovery and healing.
- Cultural, historical and gender issues - A trauma-informed approach incorporates processes that move past cultural stereotypes and biases, and incorporates policies, protocols and processes that are responsive to the cultural needs of clients.
For an example of an Australian model of trauma-informed care, see Tucci and Mitchell's (2015) outline of the basic understanding of trauma that informs appropriate care underpinning the services and training provided by the Australian Childhood Foundation: 9 Plain English Principles of Trauma Informed Care.
The Berry Street Childhood Institute also provides a number of resources and training on trauma-informed care for children.
Achieving trauma-informed services: Reflection questions for service managers
- What is the likelihood of clients who have experienced trauma accessing our service?
- Do we provide access to trauma-specific evidence-based treatments for current psychological difficulties that result from that trauma (e.g. Trauma-focused cognitive-behaviour therapy)?
- Do we provide access to effective treatments for complex trauma and complex PTSD (for which trauma-specific treatments may not be as effective)?
- (See: Connor & Higgins, 2008a, 2008b; Kezelman & Stavropoulos, 2012).
- Are these trauma-specific interventions provided inhouse, in collaboration with other agencies, or via referral to an external agency (and if so, do we provide active/warm referral)? See:
- How do we incorporate restorative justice principles?
- According to Higgins et al. (2014), restorative justice activities might include:
- addressing trauma and other mental health consequences through evidence-based therapeutic interventions;
- repairing the injuries caused to relationships, especially between sons/daughters and parents;
- providing opportunities for truth-telling, storytelling and acknowledgement; and
- overcoming shame and recognising past actions through public activities and community awareness campaigns.
- See: Higgins et al., 2014, pp. 41-46: Forced Adoption Support Services Scoping Study
- According to Higgins et al. (2014), restorative justice activities might include:
- Who in the organisation is likely to come into contact with individuals who have experienced trauma, or be providing information to, or receiving communications from clients experiencing trauma? Thinking from a "client journey" perspective, this might include:
- phone/intake staff;
- web/staff with online monitoring;
- reception;
- office manager;
- media and communications staff;
- other staff or contractors on the premises (e.g. catering, cleaning, security); and
- project/service delivery professionals and support staff.
- Who is less likely to be interacting with trauma survivors but who need to understand, and who need to support "front-line" workers and other support staff who do?
- executive staff (who create the authorising environment);
- managers and team leaders; and
- mentors and supervisors.
This suggests the value of whole-of-organisation approaches to trauma-informed service delivery, directed at every level to ensure a focus on what helps clients feel safe.
- What should training encompass? Training should include:
- skills in de-escalation or "holding" clients who are experiencing an acute episode of trauma or re-traumatisation;
- debriefing and staff protocols for responding to difficult situations and clients presenting with complex circumstances and trauma histories;
- information on staff care and preventing/responding to secondary or vicarious trauma - the psychological term for changes that can occur to people when they are repeatedly exposed to traumatic material (see Feeling heavy: Vicarious trauma and other issues facing those who work in the sexual assault field);
- organisational supports to prevent or address vicarious trauma for staff including: clinician self-care skills and reflective practice, caseload management, supervision, debriefing, staff and peer support, workplace safety, comfort and supportive work culture that acknowledges the reality of vicarious trauma (Morrison, 2007);
- types of events/circumstances in clients' lives that may be traumatising;
- typical modes of reacting - events/triggers for re-traumatisation; and
- understanding the impacts of trauma (such as behavioural symptoms typical of PTSD, as well as the developmental impacts of victimisation and trauma on an individual's beliefs - about the self, the world, and the future - e.g. see: Janoff-Bulman & Frieze, 1983).
Further to this, SAMHSA also provide a range of sample questions to consider when implementing a trauma-informed approach.
Which services should be delivering trauma-informed care?
Most of the US literature about trauma-informed care is directed at change in behavioural health services. In Australia there appears to be an emphasis on driving change in the mental health sector. This has the potential to cause confusion about the pathway to providing trauma-informed care in the child, family and community sectors and about what being trauma-informed actually means. One aspect of clarifying these questions is to understand which services should be adopting a trauma-informed approach to human service delivery.
In addition, there are communities and populations for whom violence and intergenerational trauma are a constant reality. Some Indigenous communities, for example, experience the phenomenon of trans-generational trauma whereby trauma is transmitted across a number of generations (Atkinson, 2002). The historical impacts of colonisation on Aboriginal people in Australia have played out in a history of disadvantage and discrimination as traditional Aboriginal life was gradually disrupted and dismantled (Atkinson, 2002; Keel, 2004). The effectiveness of the full range of health and human services in such communities could be enhanced by a trauma-informed approach (Atkinson, 2013).
As outlined in the earlier discussion on principles of trauma-informed care, it is important for services to be culturally attuned and relevant (Atkinson, 2013). This is described by SAMHSA as the principle that the trauma-informed organisation actively moves past cultural and gendered stereotypes and incorporates policies and processes that are responsive to the cultural needs of individuals served, including addressing historical trauma (SAMHSA, 2014) or collective trauma (Atkinson, 2013).
Building on the work of Harris and Fallot, SAMHSA's (2014) Concept of Trauma and Guidance for a Trauma-Informed Approach outlined ten implementation domains:
- governance and leadership;
- policy;
- physical environment;
- engagement and involvement;
- cross-sector collaboration;
- screening, assessment, treatment services;
- training and workforce development;
- progress monitoring and quality assurance;
- financing; and
- evaluation (p. 12).
This guidance information is designed to provide a starting point for an organisational approach to implementing trauma-informed care. It also indicates that organisations across all settings should consider how trauma-informed approaches could benefit stakeholders regardless of whether they deal with trauma in their day-to-day business. The reality of the prevalence of traumatic experiences in the general population indicates that trauma is not confined to prevention, treatment and recovery settings but is integral in other systems as well (SAMHSA, 2014).
It is important to note that many practices that service providers currently use are likely to already be consistent with a trauma-informed approach, such as conveying empathy and validating the client's experiences (Knight, 2015). What is different about identifying as a trauma-informed service is that there is a paradigm shift in service delivery culture to acknowledge and clearly articulate the importance of trauma in understanding and responding to client presentation.
With the lack of an overarching framework in Australia, there is a danger of developing trauma-informed models and practices that are not sharing a consistent language about what being trauma-informed entails. This issue is discussed in more depth in the section about challenges to implementation later in this paper.
The need for a systems approach to trauma-informed care
Following the lead of the USA, Australian health agencies are moving towards a trauma-informed paradigm for considering health and human service delivery systems (Kezelman & Stavropoulos, 2012) in preference to a medical model of individual illness (DeCanandia, Guarino, & Clervil, 2014).
The effects of traumatic experience often manifest in behaviours that result in people being involved in human service systems that go beyond mental health, such as the criminal justice system (SAMHSA, 2014). A systems approach to trauma-informed care means that implementation goes beyond individual practitioner and service organisation change to extend to whole systems that people who have experienced trauma are likely to interact with. A system, for example, could include the justice, homelessness or child welfare systems. These systems may not include treatment settings but can still affect the people who experience them. In the USA, a range of systems are in the process of adopting a cross-sectoral approach to implementing trauma-informed care and trauma-specific services to support service users (DeCanandia et al., 2014). For example, the behavioural health and health care, veterans' administration, homelessness and education sectors are just a few of the systems that are shifting to a trauma-informed approach (DeCanandia et al., 2014).
The differences between trauma-informed services and trauma-specific services are described in the definitions outlined earlier. It is important to distinguish between them but acknowledge the intersection of the two types. Trauma-specific services are designed to treat the symptoms or manifestations of the effect of a trauma on an individual but these interventions must be delivered in a trauma-informed context. This emphasises an overall philosophy of trauma as a central concept in understanding the presentation of clients within a range of health and welfare settings (Kezelman & Stavropoulos, 2012).
Challenges in implementing a trauma-informed approach to care
As noted previously, implementing trauma-informed care requires a paradigm shift in service delivery (Hopper et al., 2010; Jennings, 2004). The literature around trauma-informed care indicates that there are still some challenges to implementing this approach for systems and services, as well as the need for research to evaluate the approach's effect on client wellbeing and other service delivery outcomes (Ashmore, 2013; Australian Centre for Posttraumatic Mental Health & Parenting Research Centre, 2013; Hopper et al., 2010; Muskett, 2014). These challenges are discussed in the following sections.
Inconsistent understandings of what it means to be trauma-informed
The most identifiable challenges across the literature are in the need to create shared understandings, and current inconsistencies in education regarding trauma-informed care (Australian Centre for Posttraumatic Mental Health & Parenting Research Centre, 2013; Hopper et al., 2010). It is difficult to align organisational change to a specific practice without a shared understanding or vision of what trauma-informed care actually is. In a comparative study of trauma-informed care in acute mental health inpatient units, Ashmore (2013) identified this as an issue in the implementation of trauma-informed care in an acute patient environment. A lack of definition and of a shared framework, as well as a lack of information specific to an acute mental health inpatient setting, were associated with challenges and inconsistency in implementation.
In their review of the literature, the Parenting Research Centre and the Australian Centre for Post-traumatic Health (2013, now Phoenix Australia) found that although participants within the child and family services sector who worked with children exposed to trauma were familiar with terminology such as "trauma-informed care", they argued that:
- the field still lacked clear definitions or understandings of concepts;
- there were assumptions that children's social and behavioural difficulties were necessarily trauma-related without clear assessment; and
- there was a lack of guidelines for assessment and treatment of trauma.
SAMHSA's (2014) recent guidance document is clearly aimed at addressing this lack of consistency in definitions and the 2012 document by Adults Surviving Child Abuse provides some practice guidelines (Kezelman & Stavropoulos, 2012). However, an aspect of trauma-informed care is that it must be culturally relevant to the populations it serves (Elliot et al., 2005; Jennings, 2004) and any broad level articulation of policy approaches or frameworks must be applicable in a range of systems and settings and for a variety of cohorts.
Translating trauma-informed care to specific practice and service settings
In addition to the array of terminology and concepts that are sometimes used interchangeably and inconsistently, there is a lack of evidence-based guidance for specific settings and systems to assist with coordinating how trauma-informed practice should be provided for particular service settings and specific populations of service users. This issue was identified by Muskett (2013) and Ashmore (2013) in relation to mental health nursing, where the need to remove the use of seclusion and restraint is emphasised but, beyond this, little has been articulated to support the use of specific practices for service settings to adopt to improve service delivery consistent with principles of trauma-informed care. Dealing with survivors of trauma, particularly in a mental health or child protection setting, may require individuals to use their prior experience to respond to specific situations. In such stressful and potentially dangerous settings, crisis management could lead to a de-prioritisation of trauma-informed responses (Conners-Burrow et al., 2013). Training and guidance for staff on how to respond to acute situations appropriately and feel confident that they are acting in accordance with the principles of trauma-informed care is recommended (Knight, 2015; Muskett, 2014).
Facilitating complex system change
As noted by the American Institute for Research, in order to build a trauma-informed system, commitment at all system levels is required. This includes a commitment to ongoing training and service transformation (DeCanandia et al., 2014). Australia is behind the USA and Canada in developing models and systemwide responses to children and other service users impacted by trauma (Bateman et al., 2013). For example, the USA has the National Child Traumatic Stress Network, funded by SAMHSA, which brings a singular and comprehensive focus to responding to childhood trauma. Australia is arguably still at the stage of requiring policy change to articulate a clear direction for moving towards systems of trauma-informed care in a range of different service delivery areas relating to child/family wellbeing (Bateman et al., 2013).
Systemic change is important because it enables people to receive services that are sensitive to the impact of trauma regardless of whether they enter through any particular service setting or intervention.
Large-scale systems change is also logistically difficult and time-consuming and requires commitment and resources (Hopper et al., 2010). Philosophical differences between sectors that need to work together to integrate care can also impede systemic change (Hopper et al., 2010). Ashmore (2013) identified particular features of systems change for systems such as mental health that are challenging. These challenges include that hierarchical systems such as health may encounter resistance and that there is an inherent power inequality between service users and professionals in such environments.
Creating change at a systemic level is more than providing practitioners and organisations with tools. It requires changes to funding models to support outcomes rather than outputs, and changes to education for mental health practitioners, social workers and other specialists. Essentially, this is about a move towards a more holistic understanding of the inter-related biological, psychological and social dimensions of trauma.
Evaluating a trauma-informed approach to care
Studies from the USA, particularly following the Women With Co-Occurring Disorders Study, have found that trauma-informed, integrated services are judged to be cost-effective when compared with treatment as usual in the comparison sites of that particular study (Domino, Morrisey, Chung, Huntington, & Larson, 2005). Although this study is regularly cited in the literature as evidence of the cost-effectiveness of trauma-informed care (DeCanandia et al., 2014, Hopper et al., 2010; Kezelman & Stavropoulos, 2012); in reality, there is a lack of evaluation about cost-effectiveness and other aspects of trauma-informed care approaches, including its effectiveness in improving outcomes for service users (Quadara, 2015). There is also a lack of evaluation tools to measure the extent to which an organisation is trauma-informed, and the lack of consistent definitions further translates into difficulties in identifying a clear method to indicate the degree to which a service or program is trauma-informed (Hopper et al., 2010).
Other challenges identified in evaluating trauma-informed care, highlighted by Hopper et al. (2010), include the difficulty in measuring cultural change and sustainability of change and whether changes in outcome are attributable to trauma-informed environments or trauma-specific interventions. In addition, the need for cross-system collaboration and assessing human service interactions to establish the extent of trauma-informed care practice implementation further complicates evaluation in this area (Kramer et al., 2015).
Applying trauma-informed care principles
To illustrate how trauma-informed care principles can be applied to respond to different trauma issues, we briefly look at service delivery in the context of people affected by the policies that created the Stolen Generation, past adoption practices and humanitarian migration.
The Stolen Generation
In their program logic, the Aboriginal and Torres Strait Islander Healing Foundation (2014, p. 25) explain how a collective healing process for members of the Stolen Generation and their descendants can occur, and the mechanisms that underlie this process. Central to this model is an understanding of an Aboriginal world view and the pervasive trauma of colonisation, and the need for specific strategies to address ongoing, collective trauma. A common element of collective healing projects is that they are based on a trauma-informed or recovery framework. According to the Healing Foundation (2014):
Trauma-informed practice is a strengths-based approach to healing that: is based on an understanding of, and responsiveness to, the impact of trauma; emphasises physical, psychological, and emotional safety for people seeking help and for the helpers; and creates opportunities for people affected by trauma to rebuild a sense of control and empowerment. It recognises the prevalence of trauma and is sensitive to and informed by the impacts of trauma on the wellbeing of individuals and communities. (p. 47)
Forced adoption and past family removal practices
An example of an issue that has only recently received public acknowledgement of its role in traumatising a large number of Australians is the former practice of forced adoption, or separation from family due to past family removal practices. In their exploration of good practice principles for services addressing the needs of people affected by forced adoption and past family removal practices, Kenny, Higgins, and Morley (2015) noted:
There is increasing recognition of the potential for trauma for individuals who have been subjected to forced adoption policies and practices, and the value of a "trauma-informed" or "trauma-aware" approach to service delivery. Good practice suggests that service providers should approach all clients with a forced adoption experience as if they might be trauma survivors (p. 8).
In their overview of good practice principles, Kenny et al. (2015, p. 8) outlined the key elements of trauma-informed service delivery. Being a trauma-informed service ensures the provision of:
- a safe and supportive environment that protects against physical harm and re-traumatisation;
- an understanding of clients and their symptoms in relation to their overall life background, experiences and culture;
- continued collaboration between service provider and client throughout all stages of service delivery and treatment;
- an emphasis on skill building rather than managing symptoms;
- an understanding of the symptoms and survival responses required to cope;
- a view of trauma as a fundamental experience that influences an individual's identity rather than a single discrete event; and
- a focus on what has happened to a person rather than what is wrong with a person.6
Humanitarian migrants surviving torture and trauma
The NSW Service for the Treatment and Rehabilitation of Torture and Trauma Survivors (STARTTS) outline the program logic for their service model as systemic and based on an ecological model of factors that influence and support healing for survivors (see How We Work).
They aim to provide a range of services that reflect the bio-psycho-social model, such as:
- complementary therapies or neurofeedback to address biological impacts;
- counselling to address psychological impacts; and
- community development projects to support social changes.
"There is nothing more practical than a good theory": The theoretical basis of trauma-informed models of care
(a) Attachment - developing a secure base
Attachment theory (Bowlby, 1988) has been used by developmental psychologists to explain positive, secure relationships between infants and caregivers, and how this forms the template for secure adult interpersonal relationships. Disruption to the relationship or insecure attachment is seen as a fundamental mechanism by which childhood trauma affects adult self-concept, wellbeing and interpersonal relationships. Trauma-informed care systems provide a safe environment to expose disruption to the attachment relationship, and build new internal models and "scripts" of the self and relationships.
(b) Self-regulation and control
Social cognitive theories of self-regulation help explain how individuals respond to threatening events. Key components of many trauma-specific treatments are to help individuals to improve self-regulation, safety, security, sense of control and mastery of their environment, and modulate their emotional reactions to traumatic stimuli. Trauma-informed systems of care are aware of the ways in which programs and organisations can trigger traumatic reactions - or even inadvertently replicate the dynamics of the traumatic events/relationships - and seek to minimise them, and promote environments that facilitate positive affect regulation or "modulation".
(c) Fundamental attribution error - overestimating the personal characteristics, underestimating situational factors
Theories of social psychology have identified that humans often make what is termed the "fundamental attribution error", whereby we over-emphasise a person's personality, or internal characteristics, in explaining their behaviour, and underestimate the environmental, or situational factors, that are external influences on their behaviours (e.g. see: Jones & Harris, 1967). For clients who have experienced trauma - particularly complex trauma involving multiple injuries in the interpersonal domain - it is likely that those around them, including their families, their work colleagues and even their health/mental health professionals, are likely to attribute their interpersonal difficulties and deficits in functioning and wellbeing to an inherent personality flaw, rather than having been shaped by their environment (i.e. the external traumatic events they have endured). Creating new environments of support, and opportunities for "reprogramming" life scripts are important. But practitioners need to be open to seeing the external influences and specifically target intervention strategies to remediate the long-standing negative consequences.
Source: The title is a quote from Lewin (1952, p. 169)
Moving forward
Much of the literature identified that the paradigm shift towards implementation of a trauma-informed approach to care needed to include commitment from political leadership at all levels (Ashmore, 2013; Bateman et al., 2013; Kramer et al., 2015).
In Australia, the Mental Health Coordinating Council (Bateman et al., 2013) has articulated the requirement for a policy statement from national and state leaders endorsing the concept of trauma as a priority mental health issue and supporting the transition to a trauma-informed service system. This would ensure that there is an identifiable commitment from governments to support the need for trauma-informed service systems.
The broad dissemination of information about trauma-informed, evidence-based best practice has been identified as an important feature of developing the evidence base around trauma (Kramer et al., 2015). Development of a nationally based resource, such as SAMHSA's National Center for Trauma-Informed Care and the National Child Traumatic Stress Network, would provide an Australian-based network of information to support policy development and service delivery and to enable the use of what is currently known about trauma-informed services in different health and human service sectors. Having central resources such as these, is instrumental in shifting human service systems towards a trauma-informed approach to service delivery.7 Australia does not yet have a body with such a specific focus but extensive work has been undertaken by organisations such as the Mental Health Coordinating Council and Adults Surviving Child Abuse, among others, to help shape behavioural health policy towards incorporating an understanding of the damaging effects of trauma into policy and service delivery approaches.
Although there are some resources and tools now available to support guidance towards trauma-informed systems of care in Australia (Bateman et. al., 2013), there does not appear to be an overarching trauma framework to support a shift in a consistent way. As noted earlier, organisations in Australia have recognised the need for trauma-informed services and interventions but the current array of methods, models and interventions on offer and in use do not support a coordinated and common approach that would ensure trauma-informed has a consistent meaning and interpretation in service delivery.
Conclusion
There is growing awareness of the need, and a strong rationale for the value, of implementing a trauma-informed approach to human service delivery. Such an approach has been adopted and implemented extensively in the USA. In Australia, there is a strong push towards trauma-informed approaches to care, and recognition of the impacts of child abuse and other traumas as a driver of service need. However, there is confusion with the array of terminology used and a lack of reference to specific trauma-informed frameworks to guide the introduction of trauma-informed care in a systemic way. Despite the need, and the conceptual/theoretical rationale, it is important to acknowledge that there is limited empirical evidence to show that working systemically to be trauma aware and providing trauma-informed systems of care leads to reductions in trauma symptoms or other positive outcomes for clients.
Currently, there is no overarching policy to mandate trauma-informed care and no framework to guide evidence-based practice to transition in a systematic way to trauma-informed care in Australia. In addition, improvements to collection of research data and adoption of standardised outcome measures for evaluation would support a more systemic approach to evaluating the implementation of trauma-informed care.
There is value in capturing practice-based evidence; however, this is beyond the scope of the current paper, and would be best carried out via a systematic and rigorous approach to gathering and synthesising information from practitioners working with traumatised clients in a variety of fields - as well as the views of those in service delivery systems that are not yet trauma-informed to examine the barriers and enablers of system change. Similarly, there is a need to articulate findings from the emerging field of trauma-informed practice into concrete policy statements or frameworks that can be applied to different client groups within and across a range of service systems and settings.
References
- Aboriginal and Torres Strait Islander Healing Foundation. (2014). Muru Marri - A resource for collective healing for members of the Stolen Generations: Planning, implementing and evaluating effective local responses. Kingston, ACT: Aboriginal and Torres Strait Islander Healing Foundation. Retrieved from <healingfoundation.org.au/wordpress/wp-content/files_mf/1423532203MuruMarriSCREENsingles.pdf>.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th edition). Arlington, VA: American Psychiatric Publishing.
- Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Perry, B. D., Dube, S. R., & Giles, W. H. (2006). The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience, 256, 174-186.
- Ashmore, T. (2013). The implementation of trauma informed care in acute mental health inpatient units: A comparative study. (Masters of Public Health), Massey University, Wellington, New Zealand.
- Atkinson, J. (2002). Trauma trails, recreating song lines: The transgenerational effects of trauma in indigenous Australia. North Melbourne, Victoria: Spinifex Press Pty Ltd.
- Atkinson, J. (2013). Trauma-informed services and trauma-specific care for Indigenous Australian children. Melbourne: Australian Institute of Family Studies.
- Australian Centre for Posttraumatic Mental Health, & Parenting Research Centre. (2013). Approaches targeting outcomes for children exposed to trauma arising from abuse and neglect: Evidence, practice and implications. Melbourne: Report produced for the Australian Government Department of Families, Housing, Community Services and Indigenous Affairs. Retrieved from <www.parentingrc.org.au/index.php/resources/supporting-children-exposed-to-trauma-arising-from-abuse-and-neglect>.
- Bateman, J., Henderson, C., & Kezelman, C. (2013). Trauma-informed care and practice: Towards a cultural shift in policy reform across mental health and human services in Australia. A national strategic direction. Position paper and recommendations of the National Trauma-Informed Care and Practice Advisory Working Group. Lilyfield: Mental Health Coordinating Council.
- Bowlby, J. (1988). A secure base: Clinical applications of attachment theory. London: Routledge.
- Breslaue, N. (2009). The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma, Violence, & Abuse, 10(3), 198-210.
- Briere, J., & Jordan, C. (2004). Violence against women : Outcome complexity and implications for assessment and treatment. Journal of Interpersonal Violence, 19(11), 1252-1276.
- Briere, J., & Spinazzola, J. (2005). Phenomenology and psychological assessment of complex posttraumatic states. Journal of Traumatic Stress, 18(5), 401-412.
- Burstow, B. (2003). Toward a radical understanding of trauma and trauma work. Violence against Women, 9, 1293-1316.
- Child Welfare Information Gateway. (2012). Trauma-focused cognitive behavioral therapy for children affected by sexual abuse or trauma. Washington, DC: US Department of Health and Human Services, Children's Bureau.
- Child Family Community Australia. (2014a). Effects of child abuse and neglect for children and adolescents. CFCA Resource Sheet. Melbourne: Child Family Community Australia, Australian Institute of Family Studies.
- Child Family Community Australia. (2014b). Effects of child abuse and neglect for adult survivors. CFCA Resource Sheet. Melbourne: Child Family Community Australia, Australian Institute of Family Studies.
- Conners-Burrow, N., Kramer, L., Sigel, B., Helpenstill, K., Sievers, C., & McKelvey, L. (2013). Trauma-informed care training in a child welfare system: Moving it to the front line. Children and Youth Services Review, 35, 1830-1835.
- Connor, P. K., & Higgins, D. J. (2008a). The "HEALTH" model - part 1: Treatment program guidelines for Complex PTSD. Sexual and Relationship Therapy, 23(4), 293-303.
- Connor, P. K., & Higgins, D. J. (2008b). The "HEALTH" model - part 2: Case study of a guideline-based treatment program for Complex PTSD relating to childhood sexual abuse. Sexual and Relationship Therapy, 23(4), 401-410.
- Cook, A., Spinazzola, J., Ford, J., Lanktree, C. Blaustein, M., Cloitre, M., et al. (2005). Complex trauma in children and adolescents. Psychiatric Annals, 35(5), 390-398.
- Courtois, C. A., & Ford, J. D. (2009). Treating complex traumatic stress disorders (Adults). New York: Guilford Publications.
- Cozolino, L. J. (2010). The neuroscience of psychotherapy. New York: W.W. Norton & Company, Inc.
- DeCanandia, C., Guarino, K., & Clervil, R. (2014). Trauma-informed care and trauma-specific services: A comprehensive approach to trauma intervention. Washington: American Institute For Research.
- Domino, M., Morrisey, J., Chung, S., Huntington, N., & Larson, M. (2005). Service use and costs for women with co-occuring mental and substance use disorders and a history of violence. Psychiatric Services, 56(10) 1223-1232.
- Dube, S. R., Anda, R. F., Felitti, V. J., Chapman, D. P., Williamson, D. F., & Giles, W. H. (2001). Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the Adverse Childhood Experiences Study. Journal of the American Medical Association, 286(24), 3089-3096.
- Elliot, D., Bjelajac, P., Fallor, R., Markoff, L., & Reed, B. (2005). Trauma-informed or trauma-denied: Principles and implementation of trauma-informed services for women. Journal of Community Psychology, 33(4), 461-477.
- Evans, A., & Coccoma, P. (2014). Trauma-informed care: How neuroscience influences practice. Hoboken: Taylor and Francis.
- Finkelhor, D., Ormrod, R.K., & Turner, H.A. (2007). Poly-victimization: A neglected component in child victimization. Child Abuse & Neglect, 31(1), 7-26.
- Alexander, P. (2013). Relational trauma and disorganized attachment. In J. D. Ford, & C. A. Courtois (Eds), Treating complex traumatic stress disorders in children and adolescents: Scientific foundations and therapeutic models. New York: Guildford Publications.
- Hahn Fox, B., Perez, N., Cass, E., Baglivio, M. T., & Epps, N. (2015). Trauma changes everything: Examining the relationship between adverse childhood experiences and serious, violent and chronic juvenile offenders. Child Abuse & Neglect, In Press.
- Harris, M., & Fallot, R. D. (2001). Envisioning a trauma-informed service system: A vital paradigm shift. New Directions for Mental Health Services, 89, 3-22. doi: 10.1002/yd.23320018903
- Herman, J. (1992). Trauma and Recovery: From domestic abuse to political terror. London: Pandora.
- Higgins, D., & McCabe, M. (2001). Multiple forms of child abuse and neglect: Adult retrospective reports. Aggression and Violent Behaviour, 6, 547-578.
- Hopper, E., Bassuk, E., & Olivet, J. (2010). Shelter from the storm: Trauma-informed care in homelessness services settings. The Open Health Services and Policy Journal, 3, 80-100.
- Huntington, N., Moses, D., & Veysey, B. (2005). Developing and implementing a comprehensive approach to serving women with co-occurring disorders and histories of trauma. Journal of Community Psychology, 33(4), 395-410.
- Janoff-Bulman, R., & Frieze, I. H. (1983). A theoretical perspective for understanding reactions to victimization. Journal of Social Issues, 39, 1-17.
- Jennings, A. (2004). Models for developing trauma-informed behavioral health systems and trauma-specific services. Rockville, MD: United States Department of Health and Human Services.
- Jones, E. E. & Harris, V. A. (1967). The attribution of attitudes. Journal of Experimental Social Psychology, 3(1), 1-24. doi:10.1016/0022-1031(67)90034-0.
- Jonson-Reid, M., Kohl, P. L., & Drake, B. (2012). Child and adult outcomes of chronic child maltreatment. Pediatrics, 129(5), 839-845.
- Keel, M. (2004). Family violence and sexual assault in indigenous communities: "Walking the talk". Melbourne: Australian Institute of Family Studies.
- Kenny, P., Higgins, D., & Morley, S. (2015). Good practice principles in providing services to those affected by forced adoption and family separation. Melbourne: Australian Institute of Family Studies. Retrieved from <www.dss.gov.au/families-and-children/publications-articles/good-practice-principles-in-providing-services-to-those-affected-by-forced-adoption-and-family-separation>.
- Kezelman, C., Hossack, N., Stavropoulos, P., & Burley, P. (2015). The cost of unresolved childhood trauma and abuse in adults in Australia. Sydney: Adults Surviving Child Abuse & Pegasus Economics.
- Kezelman, C., & Stavropoulos, P. (2012). The last frontier: Practice guidelines for treatment of complex trauma and trauma-informed care and service delivery. Kirribilli: Adults Surviving Child Abuse.
- Kisiel, C. L., Fehrenbach, T., Torgersen, E., Stolbach, B., McClelland, G., Griffin, G., & Burkman, K. (2014). Consellations of interpersonal trauma and symptoms in child welfare: Implications for a developmental trauma framework. Journal of Family Violence, 29, 1-14.
- Knight, C. (2015). Trauma-informed social work practice: Practice considerations and challenges. Clinical Social Work Journal, 43, 25-37.
- Kramer, L., Sigel, B., Conners-Burrow, N., Worley, K., Church, J., & Helpenstill, K. (2015). It takes a state: Best practices for children exposed to trauma. Best Practices in Mental Health, 11(1), 14-24.
- Lewin, K. (1952). Field theory in social science: Selected theoretical papers by Kurt Lewin. London: Tavistock.
- Markoff, L., Fallot, R., Reed, B., & Elliot, D. (2005). Implementing a trauma-informed alcohol and other drug and mental health services for women: Lessons learned in a multisite demonstration project. American Journal of Orthopsychiatry, 75(4), 525-539.
- Mieseler, V., & Myers, C. (2013). Practical steps to get from trauma aware to trauma informed while creating a healthy, safe, and secure environment for children. Jefferson City: Missouri Coalition for Community Behavioral Healthcare. Retrieved from <mocmhc.org/documents/Thursday,%20October%2024/Mieseler-Myers,%20Trauma%20Informed%20Care/PRACTICAL%20STEPS%20TO%20GET%20FROM%20TRAUMA%20AWARE%20TO.pdf>
- Morrisey, J., Jackson, E., Ellis, A., Amaro, H., Brown, V., & Najavits, L. M. (2005). Twelve-month outcomes of trauma-informed interventions for women with co-occurring disorders. Psychiatric Services, 56(10), 1213-1222.
- Morrison, Z. (2007). "Feeling heavy": Vicarious trauma and other issues facing those who work in the sexual assault field (ACSSA Wrap No. 4). Melbourne: Australian Centre for the Study of Sexual Assault, Australian Institute of Family Studies.
- Morrison, Z. (2009). Homelessness and sexual assault. Melbourne: Australian Institute of Family Studies.
- Muskett, C. (2014). Trauma-informed care in inpatient mental health settings: A review of the literature. International Journal of Mental Health Nursing, 23(1), 51-59.
- National Scientific Council on the Developing Child. (2005/2014). Excessive stress disrupts the architecture of the developing brain: Working paper 3. Updated edition. Cambridge, MA: Center on the Developing Child, Harvard University. Retrieved from <www.developingchild.harvard.edu>.
- Nurius, P. S., Green, S., Logan-Greene, P., & Borja, S. (2015). Life course pathways of adverse childhood experiences toward adult psychological well-being: A stress process analysis. Child Abuse & Neglect, 45, 143-153.
- Price-Robertson, R., Higgins, D., & Vasallo, S. (2013). Multi-type maltreatment and polyvictimisation: A comparison of two research frameworks. Family Matters, 93, 84-98. Melbourne: Australian Institute of Family Studies. Retrieved from <www.aifs.gov.au/institute/pubs/fm2013/fm93/fm93h.html>.
- Price-Robertson, R., Rush, P., Wall, L., & Higgins, D. (2013). Rarely an isolated incident: Acknowledging the interrelatedness of child maltreatment, victimization and trauma. Melbourne: Child Family Community Australia, Australian Institute of Family Studies. Retrieved from <www.aifs.gov.au/cfca/pubs/papers/a144788/index.html>.
- Quadara, A. (2015). Implementing trauma-informed systems of care in health settings: The WITH study. State of Knowledge paper. Melbourne: Australian Institute of Family Studies.
- Resick, P. A., Bovin, M. J., Calloway, A. L., Dick, A. M., King, M. W., Mitchell, K. S., et al. (2012). A critical evaluation of the Complex PTSD literature for DSM-5. Journal of Traumatic Stress, 25, 241-251.
- Stathopoulos, M. (2012). Addressing women's victimisation histories in custodial settings. Melbourne: Australian Institute of Family Studies.
- Substance Abuse and Mental Health Services Administration. (2014). SAMHSA's concept of trauma and guidance for a trauma-informed approach. Rockville, MD: Substance Abuse and Mental Health Services Adminstration.
- Tucci, J. & Mitchell, J. (2015). 9 plain english principles of trauma informed care. Retrieved from <www.childhood.org.au/blog/home/2015/april/trauma-informed-care>.
- van der Kolk, B. A. (2005). Developmental trauma disorder: Toward a rational diagnosis for children with complex trauma histories. Psychiatric Annals, 35(5), 401-408.
- van der Kolk, B. (2014). The body keeps the score: Mind, brain and body in the transformation of trauma. New York: Viking.
- Van der Kolk, B., Roth, S., Pelcovitz, D., Sunday, S., & Spinazzola, J. (2005). Disorders of extreme stress: The empirical foundation of a complex adaptation to trauma. Journal of Traumatic Stress, 18(5), 389-399.
- Wall, L., & Quadara, A. (2014). Acknowledging complexity in the impacts of sexual victimisation trauma. Melbourne: Australian Institute of Family Studies.
- Whiteford, H., & McKeon, G. (2012). System-level intersectoral linkages between the mental health and non-clinical support sectors. Canberra, ACT: Commonwealth Department of Health and Ageing.
At the time of writing Liz Wall was a Senior Research Officer at the Australian Institute of Family Studies, Daryl Higgins was Deputy Director (Research) and Cathryn Hunter was a Senior Research Officer with the Child Family Community Australia information exchange at the Australian Institute of Family Studies.
The authors wish to acknowledge the valuable feedback of Cathy Kezelman, President, Adults Surviving Child Abuse and contribution of Antonia Quadara, Research Fellow, Australian Institute of Family Studies.
Cover image: © istock/ KatarzynaBialasiewicz
Wall, L., Higgins, D., & Hunter, C. (2016). Trauma-informed care in child/family welfare services (CFCA Paper No. 37). Melbourne: Child Family Community Australia information exchange, Australian Institute of Family Studies.
978-1-76016-068-5